Role of Atherosclerosis in CHD
 Cholesterol and Lipoproteins
Cholesterol and Lipoproteins
Cholesterol is a normal lipid found in the body. It is metabolised by the liver by the breakdown of saturated
fat. It is also insoluble, therefore difficult to transport around the body. To overcome this, the body combines it
with proteins with varied size, density and molecular weight, giving its name - Lipoproteins. There are two
main forms: Low Density (LDL, and also Very Low Density - VLDL) and High Density (HDL) Lipoprotein, LDL having
a higher cholesterol content. The role of LDL is found to transport cholesterol to body cells, that have LDL
receptors, and is used for synthesis of cell walls. HDL on the other hand, picks up cholesterol from body cells and
transports it back to the liver for excretion.
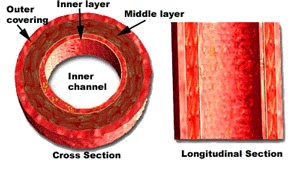
Damage
The factor that starts atherosclerosis for definite is unknown, however, the 'response to injury' idea is
widely accepted. This means, that damage to the endothelium of a coronary artery initiates the process. Damage can
be caused by toxins, hypertension, hyperglycaemia etc.
Smoking can increase platelet activity and decrease HDL levels. Hypertension and diabetes can cause endothelial
dysfunction, but hypertension can also increase endothelial permeability and monocyte accumulation. All factors to
intiate the 'injury.'
LDL readily enters arterial walls. With damaged endothelial cells of coronary arteries, LDL may accumulate in
the subendothelial/intimal layer and undergoes chemical modifications such as oxidation. Modified LDL is found to be
proinflammatory. The overall effect stimulates an inflammatory response to this site of accumulated modified LDL in
the coronary artery.
Inflammation
The inflammatory response includes increase of vascular permeability, reduced blood flow, and increased adhesive
properties of endothelial cells at the site in the artery. Circulating monocytes from the circulation diffuse through
the endothelial layer and diffrentiate into macrophages. They also secrete interleukin-1 (IL-1) and Tumour Necrosis
Factor-alpha (TNF-α). These cytokines can activate T-lymphocytes and further promote inflammation.
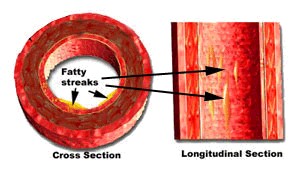
The key role of macrophages at the site of lesion is to take up the excess deposited lipid, either as
cholesterol or as LDL. This turns them into lipid-loaded 'Foam Cells' giving a characteristic yellow/grey area
in the arterial wall - also known as the 'fatty streak.'
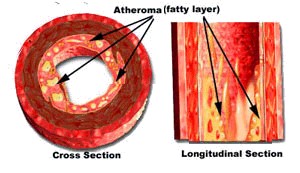
The vast combination of cytokines stimulates the proliferation and migration of smooth muscle cells from the
Tunica media to the Tunica intima, causing the site (now known as an atheroma or plaque) to become much larger.
Repair
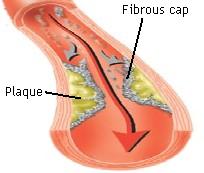
An attempt is made by the body to repair the fatty streak by covering it with a fibrous cap. It is formed by
the smooth cells that are now in the intima, by producing extracellular matrix in the forms of collagen fibres.
The cap separates the soft inner lipid core filled with macrophages, and dead cells etc. from the blood circulation.
Often, the capping is sufficient enough to prevent any further development.
The events upto this point can take place over decades, during which there may be no/very little clinical symptoms.
If the plaque is large enough to cause an unsufficient blood flow, then ischaemia results during increased physical
activity. It is clinically recognised as stable angina.
Rupture
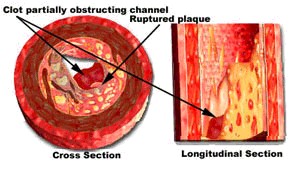
However, the fibrous cap may rupture, if for example, the cap was too thin. This allows the highly thrombogenic soft
inner lipid core to exude, so the clotting cascade becomes activated.
Platelets will stick to the site of the cap, in an attempt to seal up the rupture. The platelets release
platelet-derived growth factor (PDGF) which in combination with other growth factors will again promote the
proliferation of the vascular smooth muscle of the arterial wall.
Thrombus formation
This will, as you can imagine, cause the
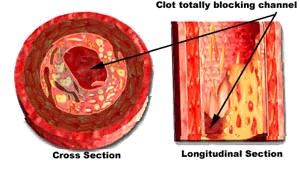
lumen diameter of the coronary artery to reduce. The thrombus has the potential to completely block the coronary artery.
A luminal occlusion of more than 50% can cause the pains of angina - in this case, unstable angina. If there is complete
occlusion, the cardiac muscle cells supplied by that branch of the artery may die, leading to myocardial infarction.
That is a Coronary Heart Disease. A disease that can start in early childhood, develop over many years and then be
clinically symptomatic in adulthood.
References [Show/Hide]

Royal Free & UCL Medical School
