Diagnosis and Investigations
Diagnosis of CHD often only takes place if there are signs of some of the less specific
symptoms such as fatigue. If risk factors also comply, then your doctor may request
you to undergo some simple tests, such as blood tests or, if neccessary a referral to a
cardiologist may be made.
In the clinic, simple physical examinations can be done which can indicate signs of a cardiovascular disease. The
doctor may
measure your weight, calculate your BMI, take an account of your lifestyle (diet, frequency of excercise etc.) and
family history.
Unfortunately, for some people, the first signs of CHD only begin to surface after periods of angina or a myocardial
infarction. After more specific investigations a definite diagnosis of CHD may be confirmed, which are outlined below.
Several investigations can be performed to assess the presence/extent of CHD. There's a diverse and varied range of
investigations that can be performed. In addition to physical examinations, the common investigations used are:
- Coronary Angiography
- 24 Hour ECG
- Echocardiogram
- Myocardial Perfusion Scintigraphy (MPS)
- Excercise Tolerance Test
- Blood Tests
Coronary Angiography

This common investigation is performed to see if there's evidence of atherosclerosis or other narrowing in the
coronary arteries. Put simply, it is an x-ray of the heart which shows blood flow through coronary arteries (the
x-ray film being known as the angiogram).
Usually performed under local anaesthetic, a catheter is inserted via the femoral artery (in the upper
leg) and fed through up to the coronary arteries. A radio opaque dye (contrast) is run through the catheter into the
coronary arteries and a series of x-ray images are taken.
More modern methods may involve a radioactive isotope (used as the contrast medium) injected via a vein in the upper
arm, see MPS.
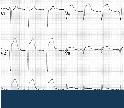
24 Hour ECG (Electrocardiogram)

There are slight variations of ECG tests. However, the principle is the same. Electrode patches are attached to your
skin and wired up to a small portable monitor which will measure the electrical impulses generated by your heart. The
monitor, such as the Holter monitor, is carried around with you for a 24 hour period during normal daily activities.
This ECG can show any abnormalities in heart function, evidence of current or previous
myocardial infarctions.
Resting ECG may be performed in combination with other tests.
Echocardiogram
Also known as 'Echo' test. This is essentially and ultrasound of your heart. A gel is applied to the chest and a
hand-held probe is used to send and pick up ultrasound waves which are then displayed on an Ultrasound monitor. This
test can be used to assess how well the heart is contracting, whether there is signs of damaged muscle/valves etc. by
how well parts of the heart moves during a contraction.
Myocardial Perfusion Scintigraphy (MPS)
This is a fairly modern technique that involves injecting a small amount of a ractioactive tracer (eg. a Thallium-201).
It is injected after a period of excercise, and then the heart is scanned under a gamma-camera. Heart muscle cells take
up the tracer from the coronary arteries. Areas that show up as defects indicate poor perfusion, and that area of cells
may be ischaemic or infarcted.
Excercise Tolerance Test (ETT)
 Commonly also known as an Excercie Stress Test.
Commonly also known as an Excercie Stress Test.
This test is a general tool of how well your heart performs during exertion, ie. during physical activity. Normally,
you will walk/run on a treadmill or pedal on an excercise bike. During which, pulse rate, ECG, blood pressure and
respiratory flow rate may be measured.
Modern ETT may also involve nuclear imaging of the heart, for example, a MPS test.
Blood Tests
Testing blood samples is often used as a routine screening tool. Common tests include:
- Cholesterol level, triglyceride level and HDL:LDL ratio to indicate plasma lipid content.
- Homocysteine test is a risk marker of vascular disorder.
- Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP) are indicators of inflammation.
- Fibrinogen levels can indicate active coagulation processes.
- Troponin I and Creatinine Kinase as indicators of recently damaged cardiac muscle or myocardial infarction.
References [Show/Hide]

Royal Free & UCL Medical School